Various theories exist as to the processes or mechanisms that may drive migraines: involving brain chemicals, blood vessels and the nervous system and it is likely to be a combination of factors, specific to each patient.
Various theories exist as to the processes or mechanisms that may drive migraines: involving brain chemicals, blood vessels and the nervous system and it is likely to be a combination of factors, specific to each patient.
‘Migraines are commonly linked to food allergy or intolerance, with detection and removal of allergens or sensitive foods eliminating or greatly reducing symptoms’.
A conventional nutrition approach is to focus on dampening down the release of inflammatory chemicals in the brain and to avoid food triggers. Certain foods containing vasoactive amines (substances like histamine, which act on blood vessels to widen them or change their permeability), can cause migraines in sensitive people.1 These include aged cheeses, chocolate, yoghurt, red wine & beer. People who are sensitive to histamine, have lower levels of the enzyme diamine oxidase, which breaks down histamine.2 Vitamin B6 is required for this enzyme to function, therefore increased intake of B6 can improve histamine tolerance, as can vitamin C.
60% of the brain is composed of fats. Reducing animal fats and increasing oily fish can alter the ratios of essential fatty acids and decrease platelet aggregation (clumping together of components of blood cells), which is thought to be a migraine trigger.3 Fish oil and olive oil are well researched to have anti-inflammatory effects and can improve migraine frequency, duration and intensity.4,5 Meat and dairy products contain an inflammatory substance called arachidonic acid, so it is advisable for migraine patients to limit these in the diet,6 replacing them with salmon, mackerel, fresh tuna, anchovies, or herring and non-dairy milk products.
Hypoglycaemia (low blood sugar) can trigger migraine7 and may occur after fasting, or after eating highly refined carbohydrates, which trigger an elevated insulin response e.g. white bread, white rice or pasta and sugary foods. Excessive sodium intake can also be linked to migraine occurrence,8 so migraine sufferers should avoid salty snacks and other processed foods.
‘Migraines are linked to liver congestion and hormonal changes, but can also be triggered by the weather, stress, hunger, perfume or lack of sleep’.
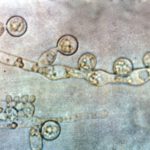
It is important to consider digestive and detoxification functions when investigating food triggers or intolerances. The toxic waste products of harmful substances in the body such as bacteria and yeasts can lead to headaches. The bacteria Helicobacter pylori has been found to be more prevalent in migraine patients compared to non-migraineurs (detected in 40% of migraine patients)9 and eradication resulted in improvements in intensity, duration or frequency for all patients.10 Presence of the bacteria can easily be tested by a GP. Suboptimal detoxification due to poor liver function; genetic issues with detoxification enzyme production; or depleted nutrients required for detoxification, can all trigger headaches.
It is useful to keep a food diary, while eliminating or being wary of common food triggers such as vasoactive amines found in: aged cheeses, chocolate, yoghurt, over ripe bananas, avocados, red plums, oranges, tomatoes, peanuts, red wine, beer and fermented foods.
Other food triggers are wheat, dairy, corn, citrus and food additives, such as monosodium glutamate (MSG), aspartame and sodium nitrate.11
MSG is found in many packaged and processed goods: potato chips and salty flavoured snacks, gravies, cold cuts of meat, condiments, soy sauce. Watch out for ingredients labelled as hydrolysed protein, autolysed yeast, glutamic acid and yeast extract.
Aspartame is used to replace sugar in low calorie or ‘light’ products such as diet fizzy drinks, as well as in flavoured milks, juices and smoothies, muesli bars, cereals, low fat yoghurts, frozen ice pops, chewing gum, sugar free sweets and also in some medication.
Sodium nitrate is a type of salt used to preserve foods, particularly meats. Found in sausages, lunch meat, bacon, ham, salami, beef jerky and smoked fish.
A variety of nutritional and herbal supplements have been researched in relation to migraine occurrence, intensity and duration, with positive effects.11-13 Supplement programmes are unique to each individual, but could include 5-hydroxytryptophan (5-HTP), vitamin B6, vitamin B2, vitamin C, magnesium, omega 3 fats, probiotics and feverfew. Contact a health professional for advice.
View List of References
1.Maintz L, Novak N (2007) Histamine and histamine intolerance. The American Journal of Clinical Nutrition, 85: 1185-1196. [Online] The American Journal of Clinical Nutrition (http://ajcn.nutrition.org).
2. Wantke F, Gotz M, Jarisch R (1993) Histamine-free diet: treatment of choice for histamine-induced food intolerance and supporting treatment for chronic headaches. Clinical and Experimental Allergy: Journal of the British Society for Allergy and Clinical Immunology, 23: 982-985. [Online] PubMed Central (http://www.ncbi.nlm.nih.gov/pmc).
3. Danese E, Montagnana M, Lippi G (2014) Platelets and migraine. Thrombosis Research, 134: 17-22. [Online] PubMed Central (http://www.ncbi.nlm.nih.gov/pmc).
4. Wagner W, Nootbaar-Wagner U (1997) Prophylactic treatment of migraine with gamma-linolenic and alpha-linolenic acids. Cephalalgia: an international journal of headache, 17: 127-130. [Online-abstract only] PubMed Central (http://www.ncbi.nlm.nih.gov/pmc).
5.Simopoulos A P (2002) Omega-3 fatty acids in inflammation and autoimmune diseases. Journal of the American College of Nutrition, 21: 495-505. [Online] PubMed Central (http://www.ncbi.nlm.nih.gov/pmc).
6.Ince H, Aydin ÖF, Alaçam H, Aydin T, Azak E, Özyürek H (2014) Urinary leukotriene E4 and prostaglandin F2a concentrations in children with migraine: a randomized study. Acta Neurologica Scandinavica, 130: 188-192. [Online-abstract only] PubMed Central (http://www.ncbi.nlm.nih.gov/pmc).
7. Necat Yilmaz, Ozgur Aydil, Aysenur Yegin, Aysun Tiltak, Esin Eren, Guzin Aykal. Impaired oxidative balance and association of blood glucose, insulin and HOMA-IR index in migraine. Biochemia Medica, 21: 145-51. [Online] (http://www.biochemia-medica.com).
8. Amer M, Woodward M, Appel L J (2014) Effects of dietary sodium and the DASH diet on the occurrence of headaches: results from randomised multicentre DASH-Sodium clinical trial. BMJ Open, 4 (12). [Online] PubMed Central (http://www.ncbi.nlm.nih.gov/pmc).
9. Su J, Zhou X-Y, Zhang G-X (2014) Association between Helicobacter pylori infection and migraine: A meta-analysis. World Journal of Gastroenterology, 20: 14965-14972. [Online] PubMed Central (http://www.ncbi.nlm.nih.gov/pmc).
10. Gasbarrini A, Gabrielli M, Fiore G, Candelli M, Bartolozzi F, De Luca A, Cremonini F, Franceschi F, Di Campli C, Armuzzi A, Ojetti V, Serricchio M, Pola R,Gasbarrini G, Giacovazzo M, Pola P (2000) Association between Helicobacter pylori cytotoxic type I CagA-positive strains and migraine with aura. Cephalagia, 20: 561-565. [Online] PubMed Central (http://www.ncbi.nlm.nih.gov/pmc).
11. Pizzorno J E, Murray M T, Joiner-Bey H (2008). The Clinicians Handbook of Natural Medicine, 2nd ed. USA: Churchill Livingstone.
12. Johnson S (2001) The multifaceted and widespread pathology of magnesium deficiency. Medical Hypotheses, 56: 163-170. [Online] PubMed Central (http://www.ncbi.nlm.nih.gov/pmc).
13. Silberstein S D (2015) Preventive Migraine Treatment. Continuum, 21: 973-989. [Online-abstract only] PubMed Central (http://www.ncbi.nlm.nih.gov/pmc).